The purpose of a surgery is to fix the root cause of an illness. If postoperative pain is neglected, or suffered in silence without being controlled, that pain is very likely to turn into long-term chronic pain. This can have a negative impact on a patient’s body, mind, and daily life.
Some people believe that “Surgery will always be a painful process,” or “Patients must endure through pain and suffer until they can’t tolerate it anymore and have to use painkillers.” These ideas not only fail to help patients, but may also delay recovery time, increase the risk of complications, and negatively impact a patient’s quality of life. There is no need to suffer through unnecessary pain.
Uncontrolled postoperative pain can lead to chronic pain
Cheng Kuang-I, director of the Department of Anesthesia at Kaohsiung Medical University Chung-Ho Memorial Hospital, said that surgery is a "destruction and reconstruction" of the body. The scalpel cuts through the body’s tissue and inevitably produces cutaneous pain at the surgical site, deep squeezing pain associated with visceral cuts, painful muscle tension and contraction, and a burning or stabbing sensation associated with small amounts of nerve damage. If the patient has a chronic disease or mental illness, the symptoms and level of pain will be more severe, and the course of treatment will be more complicated.
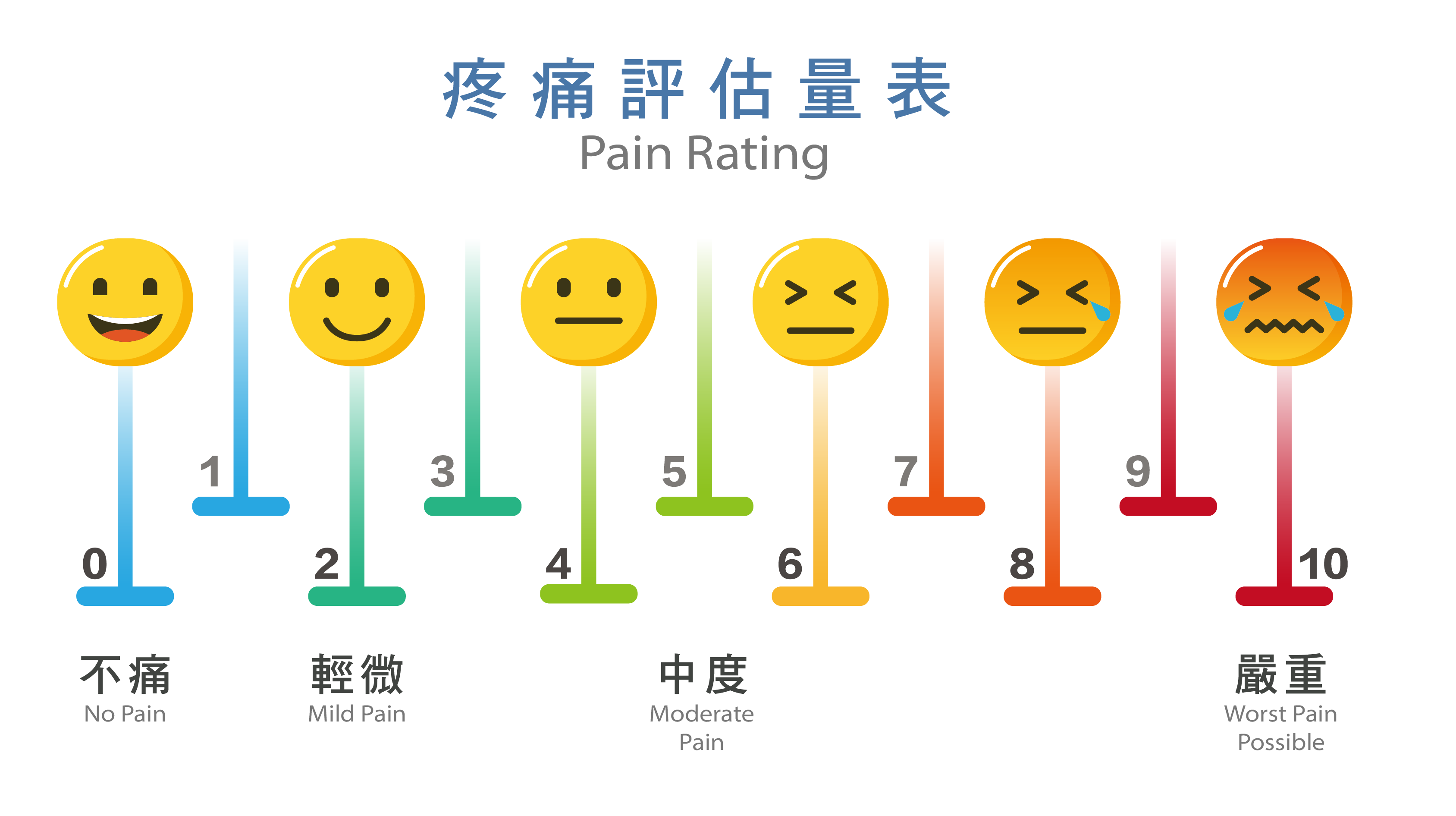
Cheng Kuang-I, director of the Department of Anesthesia at Kaohsiung Medical University Chung-Ho Memorial Hospital, said that surgery is a "destruction and reconstruction" of the body. The scalpel cuts through the body’s tissue and inevitably produces cutaneous pain at the surgical site, deep squeezing pain associated with visceral cuts, painful muscle tension and contraction, and a burning or stabbing sensation associated with small amounts of nerve damage. If the patient has a chronic disease or mental illness, the symptoms and level of pain will be more severe, and the course of treatment will be more complicated. Persistent postsurgical pain is associated with both the intensity and duration of the initial acute pain. Postoperative pain may lead to inflammation, redness, and a sensation of heat in the wound. It can also lead to a rapid heartbeat, increased blood pressure, muscle tension, abnormal endocrine and sympathetic nerve performance, etc. Some patients are afraid that breathing normally might exacerbate their pain. This results in poor lung functioning, anxiety, and mental problems, which makes the patient’s rating on the pain index even worse (Figure 1).
Patient-Centered Rethinking of Postoperative Pain Management
Safe and proper pain control is a necessary part of modern medicine and postsurgical care. Director Cheng Kuang-I said that the sensation of pain is determined by the brain. When tissue is damaged, it will transmit nerve impulses from the peripheral nervous system to the central nervous system. Reducing or blocking the transmission of this nerve impulse results in effective pain control. This can inhibit inflammation, inhibit or reduce peripheral nerve and central nerve impulse transmission, and directly inhibit or reduce the brain's nociceptive response. Common pain medications include acetaminophen (e.g., Prilosec), non-steroidal anti-inflammatory drugs (NSAIDs, e.g., diclofenac), local anesthetics, and opiate or opioid pain medications (e.g., morphine or synthetic or semi-synthetic addictive pain medications).
"In the past, postoperative pain relief was a one-man war. The surgeon or attending physician would assess the patient and prescribe a single drug. Opioid painkillers are the most commonly prescribed drug because they are very effective, but they can have serious side effects, and can even cause respiratory depression. In the past, painkillers would only be administered after a half-hour or longer process in which the patient feels pain, then notifies the nurse, who then notifies the doctor, who then prescribes the painkillers to be administered. This long process causes patients to experience unnecessary pain.
In recent years, the medical profession has promoted patient-centered ERAS (Enhanced Recovery After Surgery), which integrates surgery, anesthesiology, rehabilitation, nursing, and nutrition to provide appropriate care at each stage of surgery and recovery to prevent postoperative complications. Cheng Kuang-I said that the current trend in pain management emphasizes multimodal analgesia (MMA), which means that before, during, and after surgery, physicians combine multiple drugs, local anesthesia, or central or peripheral nerve blockage therapy to achieve immediate and sustained high-quality pain control.
"In other words, we are optimizing each method of pain treatment and controlling unnecessary side effects," he said. For example, patients undergoing knee surgery will receive a peripheral nerve block, intravenous pain medicine, and oral pain medicines to reduce the risks of side effects like drowsiness. This approach also helps initiate earlier postsurgical feeding and increases patient mobility and stamina," he said. Physicians can evaluate each case and prescribe an appropriate multimodal medication regimen to reduce dependence on a single medication and also to reduce side effects. This method of pain control is more effective.
New long-acting pain relief with fewer side effects and faster recovery
The most important thing after surgery is to recover as quickly as possible. Shortening the amount of time patients spend in pain greatly improves their recovery. Because the blood concentration of pain medication in the body fluctuates, patients have to repeatedly take more medicine as the effects of the prior dose wear off and their pain returns. Cheng added that for postoperative pain, long-acting painkillers can be used to provide background pain relief. Long-acting painkillers have a more stable blood concentration, so patients only need to take short-acting pain medicines occasionally, when they are experiencing the peak level of pain. This type of multimodal pain relief reduces side effects, reduces opioid dosages, and reduces the problems between patients and medical staff that sometimes occur in the context of opioid usage. At present, there are long-acting NSAID injections that provide effective pain relief for up to 12 hours. There is also a new type of special long-acting pain relief injection developed by Taiwanese scientists. It provides effective pain relief, similar to morphine, for up to 7 days, but with less serious side effects than morphine. This medicine is especially helpful for patients undergoing surgeries that have short hospital stays and incur moderate to severe pain, because the medicine’s pain relief will remain effective after the patient is discharged from the hospital. This speeds up their recovery time. However, because this medication’s effect has a long duration, it is recommended that a professional evaluate each patient before administering the medicine.
Cheng Kuang-I stressed: "Suffering does not mean bravery. If pain is not dealt with properly or if the recovery process extends beyond the normal timeline, intense pain will likely continue and could even cause permanent damage. Patients experiencing pain should seek medical help as soon as possible. This is the right attitude for dealing with pain.
Posted from https://www.gvm.com.tw/article/94226